By Hannah Lee
In July 2023, the Tacoma-Pierce County Health Department (TPCHD) reported that a potentially deadly fungus was confirmed in western Washington hospitals, specifically in Pierce County.
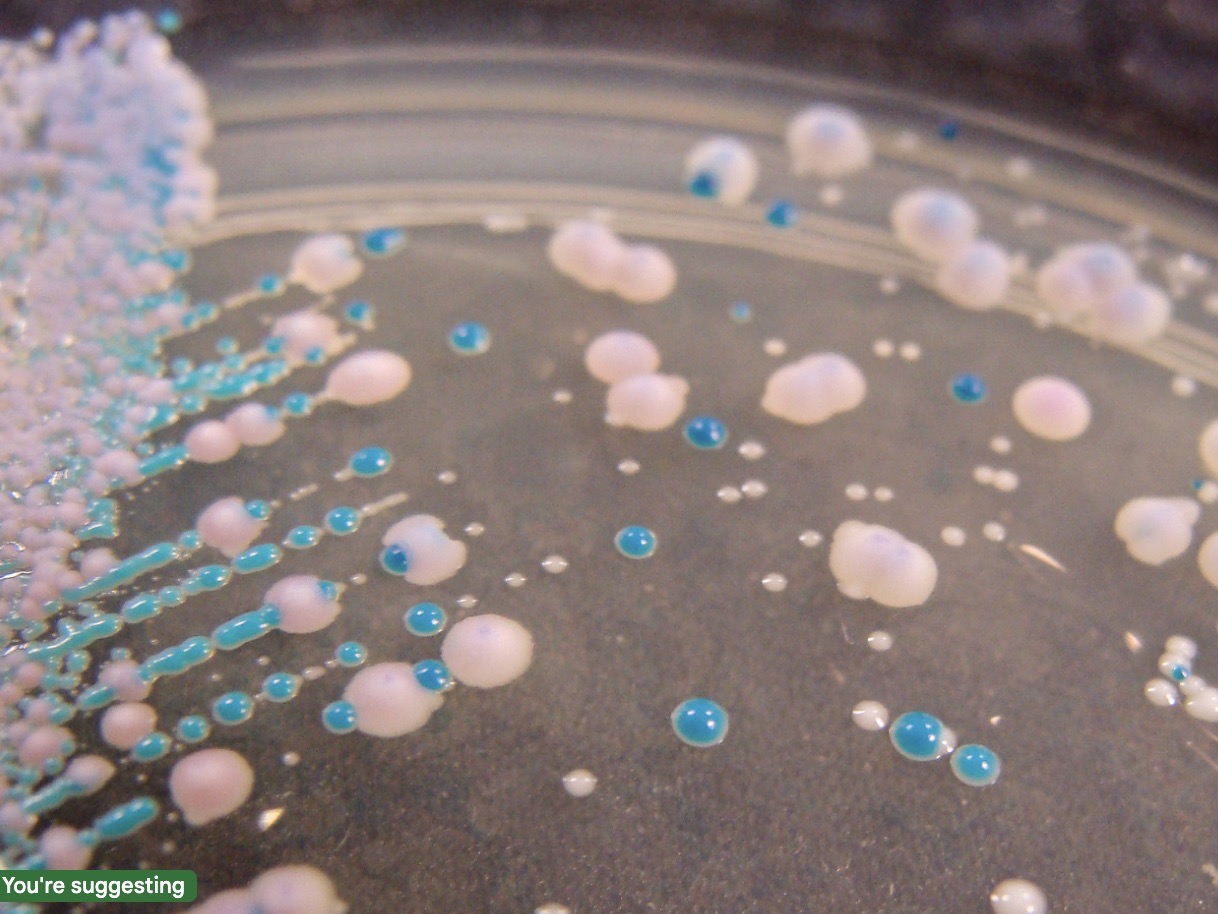
The fungus, Candida auris (C. auris), “is a type of yeast that can cause severe illness and spreads easily among patients in healthcare facilities,” per the Center for Disease Control (CDC). It often is resistant to antifungal treatments, meaning that the medications designed to kill the fungus and stop infections do not work.
King County reports that there have been four cases of C. auris infections in Washington so far. While the CDC and TPCHD did not have data for Washington state’s spread of the fungus, the CDC does have data for C. auris infections across a few states. States like Nevada and Pennsylvania reported a record-high number of infections and colonizations, which indicates a fairly rapid spread.
Symptoms can be similar to that of a bacterial infection such as fever and fatigue, and health officials do not have a list of common symptoms for C. auris infections yet. Infection entry points include the bloodstream, ears, and open wounds. The CDC notes that C. auris is the most dangerous when it becomes an invasive infection, such as via the bloodstream. They state that “many of the patients who become sick with C. auris are usually already very sick, which makes it hard to know how much C. auris contributed to their death.” The spread of C. auris happens through ‘colonized’ people. ‘Colonized’ means any person can carry C. auris on their skin and can spread it to surfaces that they are in contact with, which can ultimately lead to it spreading to others. The CDC notes that even those who are symptom-free can still transmit the infection.
There are two ways that healthcare professionals can test for C. auris infection: a colonization screening and clinical specimen testing. According to the CDC, a colonization screening is when “a healthcare provider swabs the patient’s skin by rubbing a swab near the armpits and groin and sends the swab to a laboratory for testing,” and a clinical specimen testing is when a blood or urine sample is collected from someone who is showing symptoms of infection. However, clinical specimen tests also test for many other different kinds of infection, not just C. auris. These infections only affect immunocompromised and medically complex patients, such as those with breathing tubes, feeding tubes, and catheters. Healthy people without these risk factors and healthcare workers have a low risk of being infected and a low risk of complications. However, healthy people can still be colonized with C. auris fungus.
One possible reason for C. auris’ spread is climate change. In a study published in an American Society of Microbiology magazine, Casadevell et al. proposed that C. auris grew faster in higher temperatures. It grows well at 40 degrees Celsius, or 104 degrees Fahrenheit. Global warming has warmed the earth’s temperature overall, and Casadevell and colleagues claim that that can help select which fungi clades can reproduce, especially in avian and mammalian basal temperatures. Scientists hypothesize that human contact with birds is what allowed the fungal infection to transfer from the wetlands, where the fungus originally developed, to humans.
C. auris has also proven to be resistant to all three classes of antifungal medications, so the course of treatment is usually multiple antifungal treatments or newer antifungal treatments. The CDC does not recommend that those who are ‘colonized’ get treatment as there is no evidence that this prevents sickness.
When someone is ‘colonized’ with C. auris fungus, there is a chance of it becoming a more severe threat but as mentioned earlier, healthy people becoming sick is rare. For those who are immunocompromised or have necessary external medical devices such as catheters and breathing or feeding tubes, C. auris has a higher chance of becoming severe. Some precautions that people can take are washing your hands thoroughly and often, disinfecting the room that a colonized person has been in, and limiting contact with those who are colonized. While the campus community is not at a particularly large risk currently, it’s something that the student body should be aware of and cautious about.
